A 63 year old presented with weakness
This is an online E log book to discuss our patient's d-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
Here is a case i have seen:
A 63 year old woman presented with a 1 week history of gradually progressive altered mental status.
A cheerful lady, active in preparation for her grand daughter's marriage, the attendants - her daughter, an allied care staff here in KIMS and her son - reported that developed an unusual fatigue 1 week ago, when she felt weak and was unable to function independently. She then started vomiting whatever food she took. The attendants initially felt this was a benign issue and the patient herself too was too focused on the marriage. However, things only got worse and her vomiting became persistent and she became even more weak and fatigued and required help to attend nature calls too. One day before presentation, the patient almost moribund and couldn't function at all without help - she required help with eating, going to the bathroom and even getting up from bed. The daughter recalls that she had a fluctuating course in her mentation and reported a classical mild improvement in her sensorium often in the evenings. The attendants both noticed that she couldn't hold a proper conversation and even couldn't properly understand their words or questions.
This morning, things took a turn for the worse, when she couldn't respond at all to their repeated concerned advances. She was brought to the hospital in this state. The attendants can't recall any history of urinary incontinence or involuntary movements of her limbs, they deny a history of fever, headache or photophobia, they deny any focal weakness or any illicit substance use.
The attendants deny any significant past medical history, except for hypertension for 15 years, for which she has been taking Tab TELMISARTAN 40mg + HYDROCHLOROTHIAZIDE 12.5mg for more than 10 years now. She adheres well to a salt restricted diet and takes her meds on time.
Personal history:
Appetite: lost
Bowels: constipation since 3 days
Bladder- normal micturition
Family history:
No history of DM, HTN CAD, CVA, asthma in the family
General examination: patient is conscious, coherent, cooperative
No pallor, icterus, cyanosis,clubbing,lymphadenopathy, edema.
Vitals:
Temperature: 98.9F
Pulse: 82bpm
Respiratory rate: 19cpm
Bp: 150/70mm hg
Spo2: 98% at RA
GRBS: 87 mg%
Systemic examination:
Cvs: S1 S2 heard, no additional sounds or murmurs.
Rs:Bilateral air entry present, NVBS
Per Abdomen: soft,non tender,non palpable
Cns:NAD
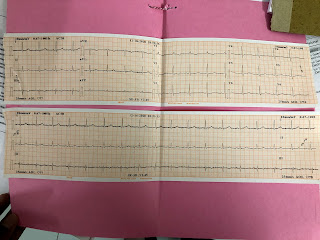
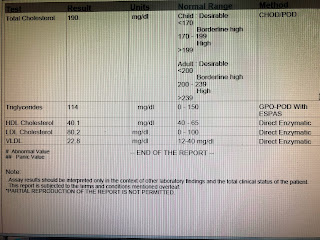
INVESTIGATIONS:
Treatment:
Day 0
Bp charting 2nd hourly
Sr.Sodium 4th hourly
GRBS charting 2nd hourly
Monitor urine output 2nd hourly
IVF -3% NaCl infusion @25ml/hr
Inj pantoprazole 40 mg iv od
Inj zofer 4 mg iv tid
Absolute free water restriction
.
Day 1:
IVF 3% Na Cl @25 ml/hr
Inj Pantop 40 mg iv od
Inj zofer 4 mg iv tid
BP,PR MONITORING
GRBS monitoring 4th hourly
Serum Sodium every 6th hourly
Fluid restriction
Allow oral soft diet
Tab MVT od
Stop all other oral medications
Day 2:
IVF 3% Na Cl @25 ml/hr
Inj Pantop 40 mg iv od
Inj zofer 4 mg iv tid
BP,PR monitoring
GRBS monitoring tid
Fluid restriction
Allow oral soft diet
Tab MVT od
Syp Lactulose 10ml/tid
Day 3:
Fluid restriction
Inj Pantop 40 mg iv od
Inj zofer 4 mg iv tid
BP,PR monitoring
GRBS monitoring tid
Fluid restriction
Allow oral soft diet
Tab MVT od
Syp Lactulose 10ml/tid
Day4:
Fluid restriction
Tab.pantop 40 mg iv od
Inj zofer 4 mg iv bd
Syp lactulose 10 ml/tid
Tab MVT po od
BP,PR monitoring
GRBS monitoring tid
Inj Optineuron 1 amp in 100 ml NS IV OD
Syp Aristozyme 10 ml/tid





















Comments
Post a Comment